Comparison Between Regular Socket and Dry Socket: Visual Guides, Signs, and Recovery Periods
Tooth extraction is a common dental procedure, but it can sometimes lead to a complication known as dry socket, or alveolar osteitis. This condition affects the healing process of the socket, causing prolonged pain and discomfort.
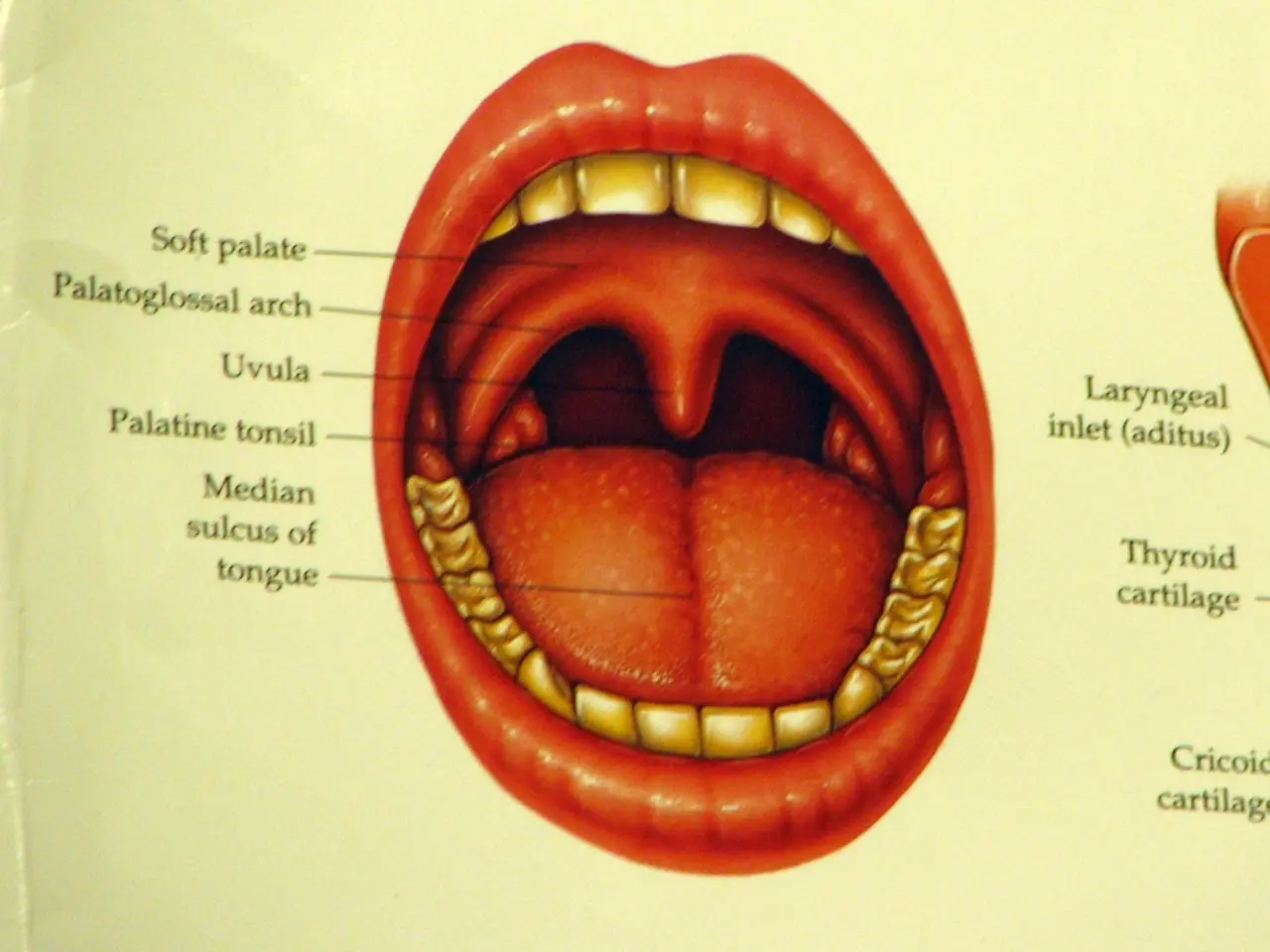
Healing Process of a Typical Socket
In a typical scenario, a blood clot forms in the socket immediately after tooth extraction, acting as a protective barrier over the underlying bone and nerves. The clot solidifies and remains intact, allowing the wound to heal smoothly. Most of the healing occurs within the first week, with significant progress by Day 7, and complete recovery by the end of two weeks. As the clot dissolves, granulation tissue forms, which is eventually replaced by bone tissue, leading to a fully healed socket.
Healing Process of a Dry Socket
However, a dry socket occurs when the blood clot either fails to form or is dislodged prematurely, exposing the bone and nerves to air, food, and fluids. Without the protective clot, healing is delayed. The exposed bone and nerves cause significant pain, often described as a deep, throbbing ache that may radiate to other parts of the face. The pain associated with a dry socket typically starts around Day 3 or 4 post-surgery and can persist longer than typical extraction pain, as it is not easily managed by standard pain medication.
Treatment for a dry socket focuses on reducing pain and may involve a dentist flushing the socket with a medicated mouthwash or saline and filling the socket with a medicated dressing. Recovery may take longer than expected due to the complications.
Risk Factors and Prevention
Certain risk factors increase the likelihood of developing a dry socket, including pressure on the wound, location and type of extraction, preexisting infection, history of serious illness and cancer, smoking, and birth control pill usage. It is important to follow the dentist's advice regarding post-surgery care, such as avoiding smoking, which can disrupt blood clot formation and the healing process.
If you experience worsening or severe pain after a tooth extraction, it is crucial to speak with a dentist. New or worsening swelling a few days after surgery, pus, fever, or pain that does not respond to pain medication are signs that may indicate an infection following a tooth extraction.
In most cases, adults can take nonsteroidal anti-inflammatory drugs, such as ibuprofen, for pain relief. However, if the pain persists or worsens, it is essential to seek professional help.
[1] Mayo Clinic [2] Colgate [3] WebMD [4] Cleveland Clinic
- In the context of NSCLC (non-small cell lung cancer), some studies are focusing on using GLP (glypse- Lincoln peptide) as a predictive biomarker for cancer treatment response.
- Regular oral health check-ups and maintaining good oral hygiene practices are crucial to preventing accidental falls and dental procedures complications in people with type 2 diabetes.
- However, some scientific research has linked type 2 diabetes to increased risks of dry socket after dental procedures, highlighting the importance of taking necessary precautions.
- In the health-and-wellness community, professional advice and proper post-surgery care are emphasized to minimize the risk of dry socket and ensure a smooth healing process.
- A study in a scientific journal suggests that good oral health significantly reduces the chances of developing atherosclerosis, a cardiovascular disease associated with diabetes.