Connection between ACPA and Rheumatoid Arthritis: Crucial Facts
Rewritten Article:
Rheumatoid Arthritis (RA) is a condition that occurs when the immune system attacks the body's own tissues, causing painful and inflamed joints. The immune system produces anti-citrullinated protein antibodies (ACPAs) to target specific proteins that have undergone a process called citrullination.
The presence of ACPAs can help doctors diagnose early signs of RA and predict its progression, including the likelihood of bone erosion. ACPAs are seen as a biological sign, or biomarker, of RA. However, not everyone with high ACPA levels necessarily has RA, as levels of rheumatoid factor (RF), another antibody, may also indicate RA. Doctors may take both ACPA and RF levels into account when diagnosing RA, as they can provide insights into disease progression and outlook.
For instance, if an individual tests positive for both ACPA and RF, they may exhibit more aggressive symptoms of RA. On the other hand, if someone only tests positive for ACPA but not for RF, they might have early signs of RA or a higher risk of developing RA. However, if both ACPA and RF tests come back negative, the individual may still have RA based on other criteria or symptoms, and they may develop ACPAs over time.
It's also important to note that if tests are positive for ACPAs and RA, the individual may have a different autoimmune condition, such as systemic lupus erythematosus (SLE) or Sjogren's disease, though this is rare.
The distinction between ACPA-positive and ACPA-negative RA can lead to different disease progression. A 2022 study found that those with ACPA-positive RA had consistently low levels of joint inflammation during periods of remission, while those with ACPA-negative RA responded better to treatment with disease-modifying antirheumatic drugs (DMARDs) in the first year of therapy. Additionally, people with ACPA-positive RA who move into remission have significantly lower inflammation levels from the point of diagnosis onward, compared to those with ACPA-negative RA.
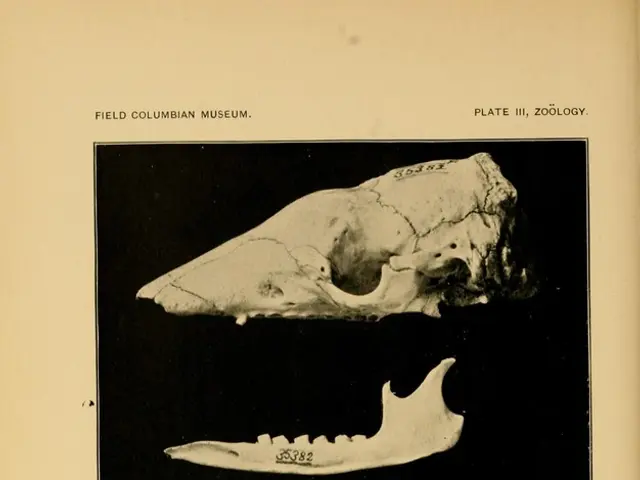
Research suggests that ACPA-positive RA may also exhibit more severe bone damage, especially in the fifth metatarsophalangeal joint, or little toe joint. Some studies have found that the scores tracking bone erosion are 3.7 to 4.4 times higher in the group with ACPA-positive RA.
Environmental factors like smoking may influence the development of RA for both ACPA-positive and ACPA-negative individuals, but smoking appears to have a greater impact on ACPA-positive RA.
The immune system produces ACPAs in response to citrullination, a process in which the enzyme peptidyl-arginine deiminase (PAD) converts arginine, a protein building block, into citrulline. While citrullination is a normal process, it happens too much in people with RA, particularly with regard to collagen, an essential component of connective tissue, tendons, and ligaments affected by RA. Cell damage can cause PAD to work too hard, leading to excess citrullination and an immune response that attacks the citrullinated proteins, bringing about another cycle of cell damage and increased inflammation.
Doctors can identify ACPAs using a blood test for CCP antibodies, a type of ACPA. This blood test usually takes no more than 5 minutes. However, it's important to note that other conditions like SLE, Sjogren's disease, tuberculosis, and chronic lung disease can also lead to raised CCP antibody levels. A doctor will consider other factors when diagnosing RA, not just the results of the blood test. Additional tests like antinuclear antibody, C-reactive protein, RF, synovial fluid analysis, X-rays, and analyzing an individual's medical history and physical exam may also be necessary.
In conclusion, ACPAs play a crucial role in diagnosing RA and predicting the course of the disease. While ACPA-positive and ACPA-negative RA may have differing disease progression and response to treatment, it is essential that individuals get proper evaluation and care from a healthcare provider to make an accurate diagnosis and develop an effective treatment plan.
- Rheumatoid Arthritis (RA) is a medical condition that arises when the immune system, instead of protecting the body, attacks its own tissues, leading to musculoskeletal problems like painful and inflamed joints.
- One way scientists identify RA is by detecting anti-citrullinated protein antibodies (ACPAs) in the blood, as they are a biomarker for RA. However, not everyone with high ACPA levels necessarily has RA, as levels of rheumatoid factor (RF) may also indicate RA.
- Understanding the presence of ACPAs can help doctors diagnose early signs of RA, predict its progression, and tailor treatment strategies, as ACPA-positive RA may respond differently to chronic diseases like RA compared to ACPA-negative RA.
- Health-and-wellness professionals should remain vigilant about the effects of chronic diseases like RA on the body, such as the potential for severe bone damage, especially in the fifth metatarsophalangeal joint, for individuals with ACPA-positive RA.