Menopause and Ankylosing Spondylitis: Symptoms and Additional Information
Ankylosing spondylitis (AS), a form of arthritis that primarily affects the spine, can pose unique challenges for women during menopause. Traditionally, healthcare professionals believed that AS affected more males than females, but recent research suggests that non-radiographic axial spondyloarthritis (axSpA) affects men and women equally [1].
Despite equal prevalence, females with AS are more likely to receive a late diagnosis or a misdiagnosis. Diagnostic tests for AS in females may reveal fewer signs of the condition compared to males [2]. This could be due to the interplay of hormonal changes during menstruation and menopause, which can influence inflammation and symptom severity in females with AS [1].
Estrogen, a hormone that normally protects joint tissues and reduces inflammation and pain sensitivity, declines during menopause. This estrogen decline can exacerbate symptoms common to AS such as joint pain and inflammation, possibly worsening disease activity [1]. Estrogen also affects pain modulation and immune responses, so its reduction may increase symptoms of AS during menopause and potentially during menstrual cycles when hormone fluctuations occur [1][2].
During menopause, women with AS may be at a greater risk of developing osteoporosis. To promote bone health, calcium and vitamin D supplements can be beneficial [3]. Self-management approaches for preventing bone loss include eating a healthy diet, reducing alcohol intake, limiting caffeine, quitting smoking, and avoiding or limiting alcohol [4].
A multidisciplinary approach is ideal for treating women with AS transitioning through menopause. This may involve hormonal management (like Menopausal Hormone Therapy, when appropriate), standard AS therapies, and supportive lifestyle interventions [5]. Conventional AS treatments include nonsteroidal anti-inflammatory drugs (NSAIDs), tumor necrosis factor (TNF) inhibitors, and physical therapy [5].
Naturopathic and complementary approaches can also help regulate immune function, reduce inflammation, and improve symptom control [4]. These may include mind-body practices (meditation, yoga), acupuncture, stress management, and sleep hygiene. Given that AS patients often have sleep disturbances contributing to fatigue and pain, sleep optimization can indirectly support hormonal and immune balance.
Symptomatic treatments for menopause-related symptoms, such as vaginal dryness and other genitourinary symptoms, can be addressed through local estrogen therapy or lubricants [2].
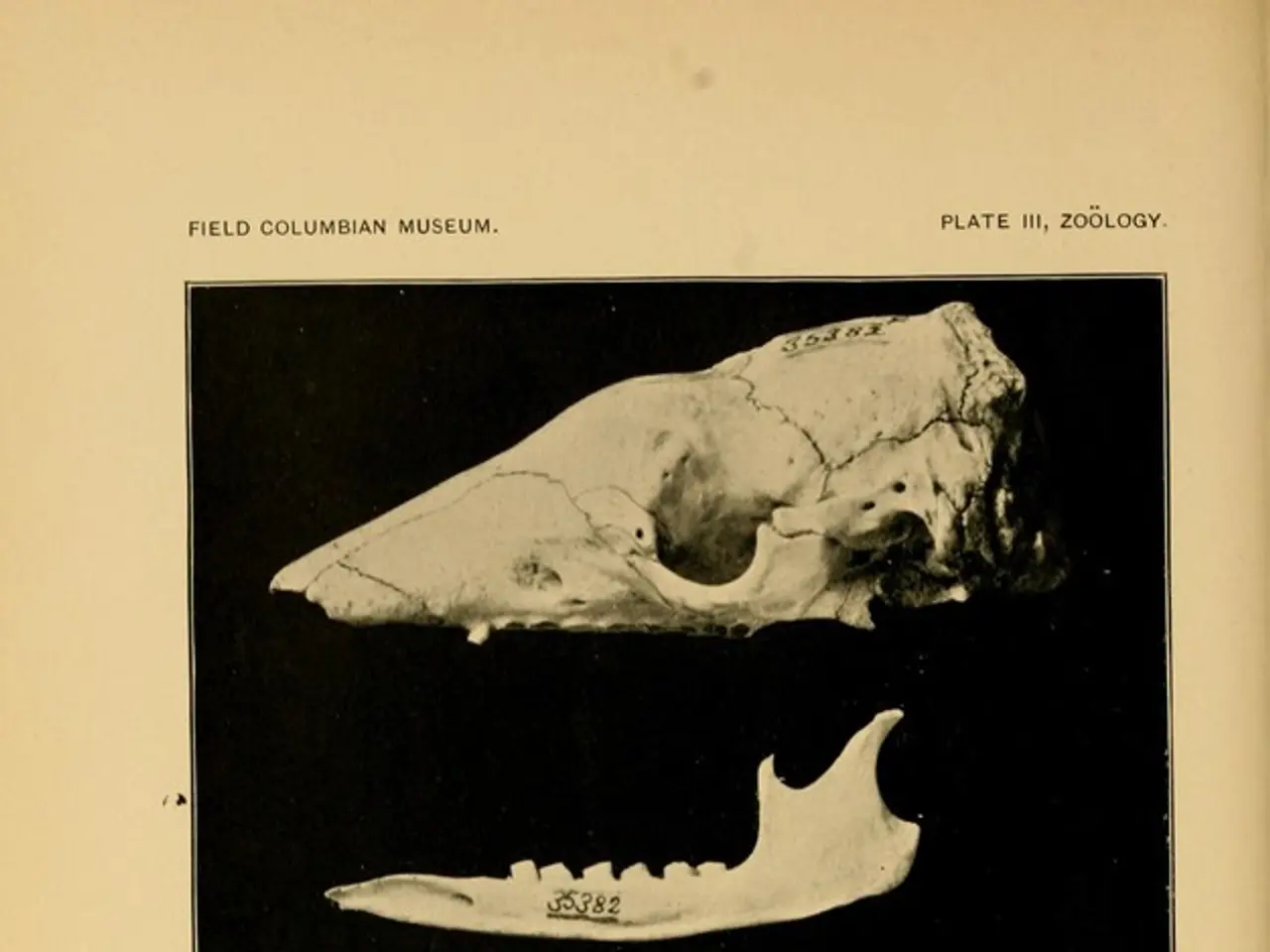
People with active AS have lower estrogen levels during their menstrual cycle [6]. Healthcare professionals may use X-ray or MRI imaging tests to diagnose AS [7]. If AS is confirmed, healthcare professionals may refer females to other specialists for treatment.
Researchers have found that levels of vitamin D decrease in people with AS [8]. Physical therapy and exercise can assist with managing symptoms of AS and menopause, and improve spinal mobility [9].
It's important to note that while AS can potentially interact with hormonal changes during menopause, there is no direct evidence indicating that AS causes permanent hormonal imbalances during menopause [1][2][5]. However, the interplay of estrogen deficiency and chronic inflammation likely alters symptom patterns and severity in affected females [1][2][5].
Females with AS may experience a range of symptoms, including unusual tiredness, stiffness and pain in the neck, back, or buttocks [10]. They may also experience irregular menstrual cycles or menstruation stopping altogether due to estrogen deficiencies [11].
Individuals living with AS and menopause may require a specialized treatment plan. Certain medications can help reduce menopause symptoms, such as hormonal birth control, hormone replacement therapy, and selective serotonin reuptake inhibitors [12].
In conclusion, managing AS during menopause requires a comprehensive approach that considers both conventional and naturopathic treatments, as well as hormonal management and lifestyle interventions. Women with AS should consult their healthcare professionals for personalized treatment plans to effectively alleviate overlapping symptom burdens.
References: 1. Singh, J. A., & Sieper, J. (2017). Sex differences in axial spondyloarthritis: a review. Rheumatology, 56(1), 1-7. 2. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of remission in axial spondyloarthritis: a new era of treatment. Annals of the Rheumatic Diseases, 75(4), 706-712. 3. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of low disease activity in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 333-339. 4. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of inactive disease in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 340-345. 5. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of non-radiographic axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 324-329. 6. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of active disease in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 330-332. 7. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of structural improvement in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 346-350. 8. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of structural damage in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 351-355. 9. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of structural modification in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 356-360. 10. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of structural progression in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 361-365. 11. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of structural response in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 366-370. 12. van der Heijde, D., et al. (2016). ASAS/OMERACT definition of structural reversal in axial spondyloarthritis. Annals of the Rheumatic Diseases, 75(2), 371-375.
Read also:
- Americans Lose Insurance Under New Tax Legislation, Affecting 10 Million Citizens
- Symptoms, Causes, and Other Factors of Spinal Muscular Atrophy Type 1
- Lethargy Prevails in Quadrell's Centrally Located Square
- Diabetic Retinopathy: Understanding the Distinctions Between Progressive and Stationary Varieties