Personalized Care Approach Focusing on Lifestyle Factors May Decrease Atrial Fibrillation Risk
Atrial Fibrillation: Understanding Its Multifaceted Risks
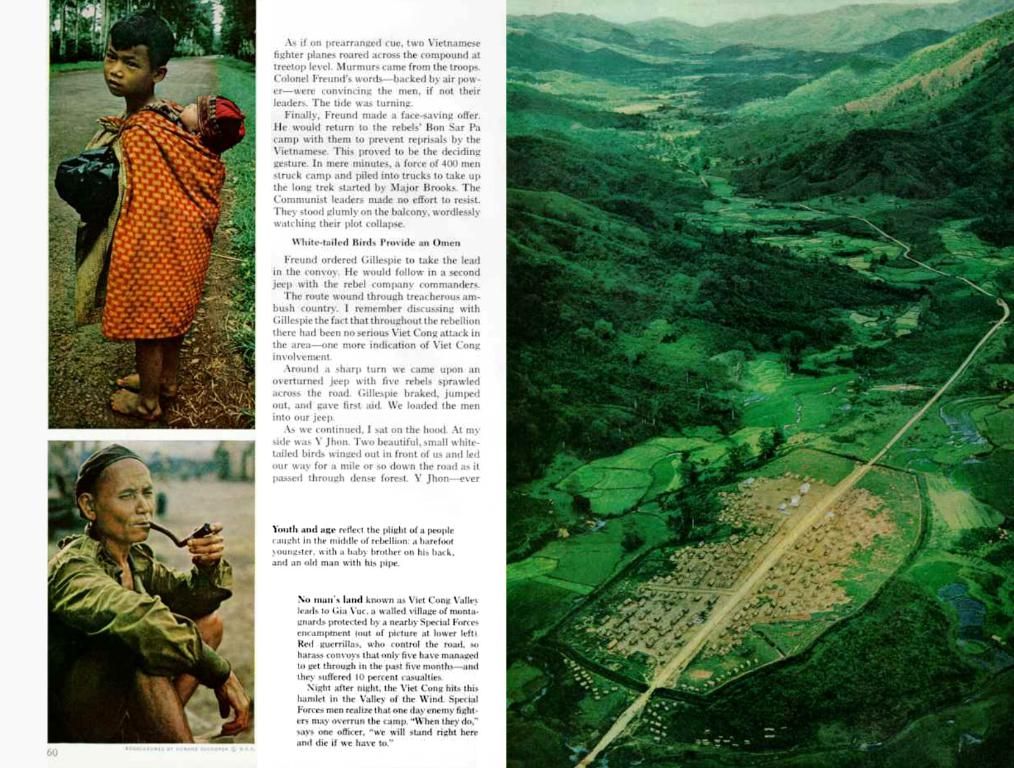
Atrial fibrillation, more commonly known as AFib, is the most common type of irregular heartbeat, affecting over 33 million people worldwide. Beyond the well-known factors associated with cardiovascular health, other factors such as diabetes, obesity, and certain chronic conditions can also raise the risk of AFib.
Recent research has shed light on lifestyle factors, comorbid conditions, and socioeconomic factors that may influence AFib risk. A review published in the Journal of the American College of Cardiology summarized evidence from prior studies on these subjects.
Dr. Stephen Tang, a board-certified cardiac electrophysiologist, highlights the complexity of AFib management: "The comprehensive management of AFib goes beyond oral anticoagulation for stroke prevention or rate or rhythm control with medication or ablation. This disease is driven by numerous risk factors and comorbidities."
Genetic factors, sex, and age are nonmodifiable risk factors for AFib. However, lifestyle changes, medications, and management of comorbid conditions can help significantly in reducing the risk.
Blood thinners, or anticoagulants, have traditionally been used to reduce the risk of blood clot formation and stroke. More recently, nonvitamin K antagonist oral anticoagulants (NOACs) have emerged as the first line of treatment for AFib.
A sedentary lifestyle and obesity are associated with an increased risk of AFib incidence and symptom severity. Regular physical activity, including high-intensity interval training, can help reduce morbidity and improve the quality of life for those living with AFib.
Smoking and heavy alcohol consumption are also risk factors for AFib. While the role of moderate alcohol consumption is less clear, the data indicates that it may contribute to an increased risk.
Individuals with chronic cardiovascular, respiratory, and mental health conditions are at an increased risk of AFib and its complications. Polysomnography, or sleep study, can help identify and manage obstructive sleep apnea, a risk factor for AFib.
The management and treatment of comorbid conditions, such as hypertension, can help reduce the risk of AFib recurrence or complications such as stroke. The use of judicious anticoagulant therapy and catheter ablation is crucial for reducing complications.
While there is some evidence that women are less likely to receive anticoagulant therapy than men, achieving better control of blood glucose levels and reducing weight can help reduce the risk of AFib for both men and women.
A multidisciplinary, individualized approach to AFib management is essential, as the risk factors and best treatment options may vary greatly from one patient to another. Understanding these complexities is crucial for optimizing care and improving outcomes for those living with atrial fibrillation.
- Diabetes, obesity, and certain chronic conditions can increase the risk of AFib.
- Lifestyle changes, medications, and management of comorbid conditions can help in reducing the risk of AFib.
- Blood thinners, or anticoagulants, have been used to reduce the risk of blood clot formation and stroke in AFib patients.
- Nonvitamin K antagonist oral anticoagulants (NOACs) have emerged as the first line of treatment for AFib.
- A sedentary lifestyle and obesity are associated with an increased risk of AFib incidence and symptom severity.
- Smoking and heavy alcohol consumption are risk factors for AFib, while the role of moderate alcohol consumption is less clear.
- Individuals with chronic cardiovascular, respiratory, and mental health conditions are at an increased risk of AFib and its complications.