Scleroderma: Characteristics, classifications, root causes, and therapeutic approaches
In the United States, approximately 75,000-100,000 people live with scleroderma, an autoimmune connective tissue disorder. While the exact cause of scleroderma remains unknown, it is believed to be an autoimmune condition that causes the body to produce too much connective tissue.
Most people who develop scleroderma are women aged 30-50 years, and the condition affects people of all ethnicities. However, recent studies suggest that African Americans may experience a more severe form of the disease.
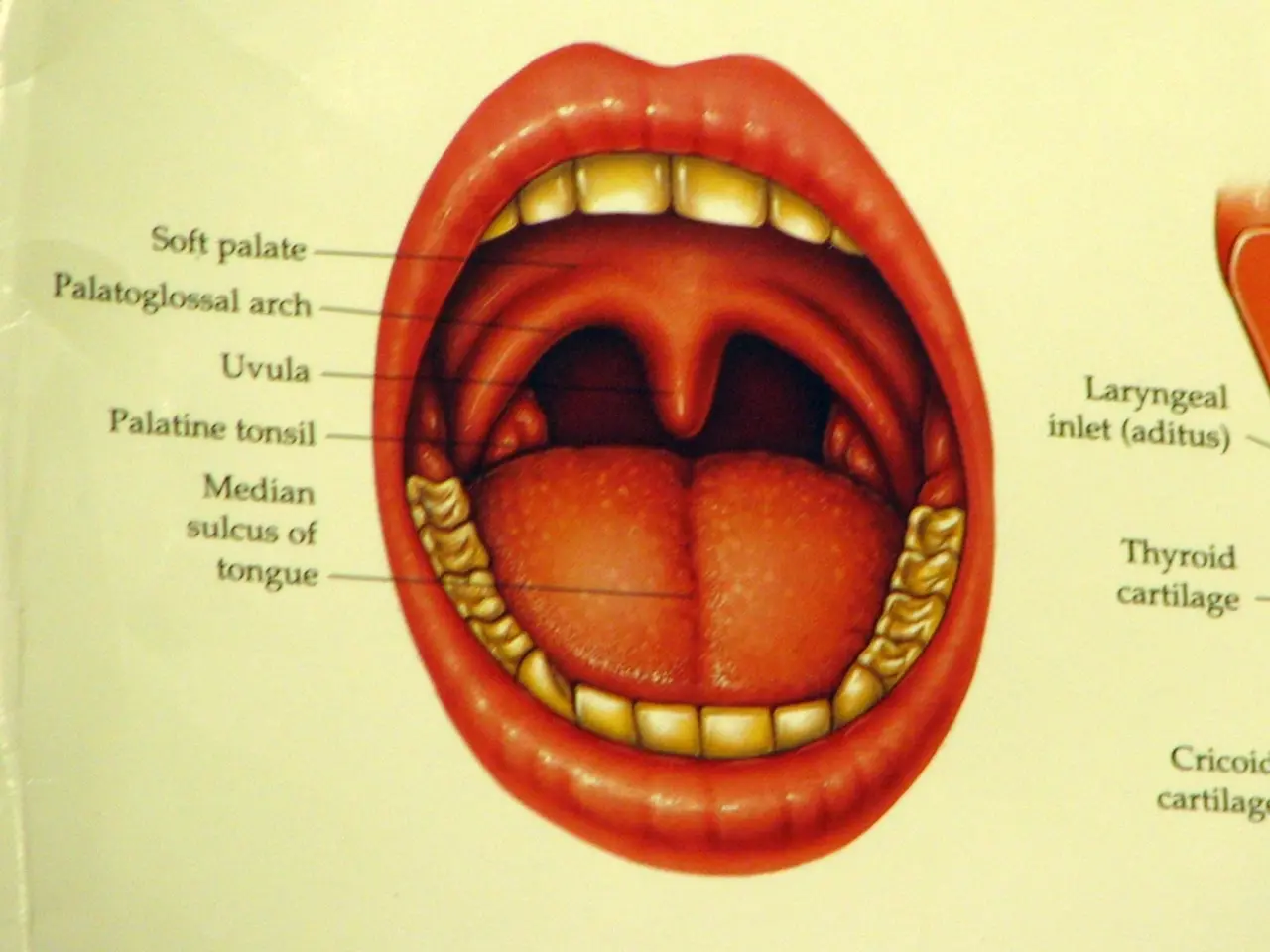
Scleroderma presents in two main types: localised and systemic. Localised scleroderma primarily affects the skin, while systemic scleroderma can affect the whole body, including internal organs. In African Americans diagnosed with systemic scleroderma (SSc), the most common symptoms and complications include both skin and internal organ manifestations.
Common symptoms in African Americans with scleroderma include skin hardening and scarring, leading to thickened, tight skin, and digital ulcers, about 50% of patients developing painful sores on fingers or toes. Fatigue and shortness of breath are also common, often related to lung involvement.
The most severe complications in African Americans with scleroderma include pulmonary, renal, and cardiac involvement. Pulmonary complications, such as interstitial lung disease (ILD) and pulmonary hypertension (PH), are common and can lead to progressive scarring of lung tissue, respiratory impairment, and breathlessness and fatigue.
Scleroderma renal crisis (SRC) is a life-threatening complication characterised by sudden onset of severe hypertension and kidney failure. In African Americans, SRC tends to be more frequent and severe. Heart complications due to fibrosis and vascular damage can occur, and are a significant contributor to mortality in scleroderma.
Research shows that African American patients with scleroderma have different antibody profiles, which influence clinical manifestations. For instance, the presence of anti-Scl-70 antibodies is associated with worse lung fibrosis, while anti-centromere antibodies are less common and linked to a lower risk of lung fibrosis.
Early recognition and management of these complications are critical to improving outcomes in this population. Scleroderma is not contagious, and a physical examination, skin tests, blood tests, and biopsies are used for diagnosis.
While there is no cure for scleroderma, treatment aims to relieve symptoms, prevent the condition from worsening, and manage complications. Management strategies include eating smaller meals, keeping skin well-moisturized, wrapping up warm, doing exercise, avoiding tobacco, alcohol, caffeine, and recreational drugs, getting enough sleep, minimizing stress, staying well-hydrated, and seeking support from the Scleroderma Foundation and the Scleroderma Education Project.
It is important to note that the outlook for scleroderma depends on the type and severity of the condition, but in many cases, it does not impact overall life expectancy. Scleroderma symptoms may include pain, stiffness, swelling, and tightness in the fingers, hands, or feet.
In the Choctaw Native American community in southeastern Oklahoma, there is a higher risk of developing scleroderma. As research continues, understanding the genetic and environmental factors contributing to scleroderma in different populations may lead to targeted treatments and improved outcomes for all those affected by this condition.
- The immune system, along with other autoimmune disorders, plays a significant role in the development of scleroderma, a chronic disease affecting health-and-wellness.
- Scleroderma is a systemic autoimmune connective tissue disorder, presenting in two main types: localised and systemic, which can affect various medical-conditions including the skin, lungs, kidneys, and heart.
- Recent studies suggest that African Americans may experience a more severe form of systemic scleroderma (SSc), with symptoms like skin hardening, digital ulcers, fatigue, and shortness of breath.
- In dermatology, skin care is crucial for managing scleroderma symptoms, while science seeks to comprehend the immune responses behind this autoimmune disorder.
- Mental health is also important in managing scleroderma, as the condition can be stressful and challenging, and support from organizations like the Scleroderma Foundation and the Scleroderma Education Project can be beneficial.
- While there is no cure for scleroderma, early recognition and management of complications, combined with lifestyle adjustments such as healthy eating, exercise, avoidance of harmful substances, and stress management, can help improve outcomes for those affected by this condition.